Is Bariatric Surgery Right for You? A Surgeon’s Guide to Sleeve Gastrectomy
Is Bariatric Surgery Right for You? A Surgeon’s Guide to Sleeve Gastrectomy
Is Bariatric Surgery Right for You? A Surgeon’s Guide to Sleeve Gastrectomy
Obesity is a growing health crisis, not only affecting physical appearance but significantly increasing the risk of diabetes, heart disease, sleep apnea, infertility, and even some cancers. When lifestyle changes and medication aren't enough, bariatric surgery, especially the popular sleeve gastrectomy, becomes a transformative option.
In this guide, we explore who qualifies for a gastric sleeve, what the procedure entails, recovery timelines, and why it's one of the most performed laparoscopic surgeries in the world today.
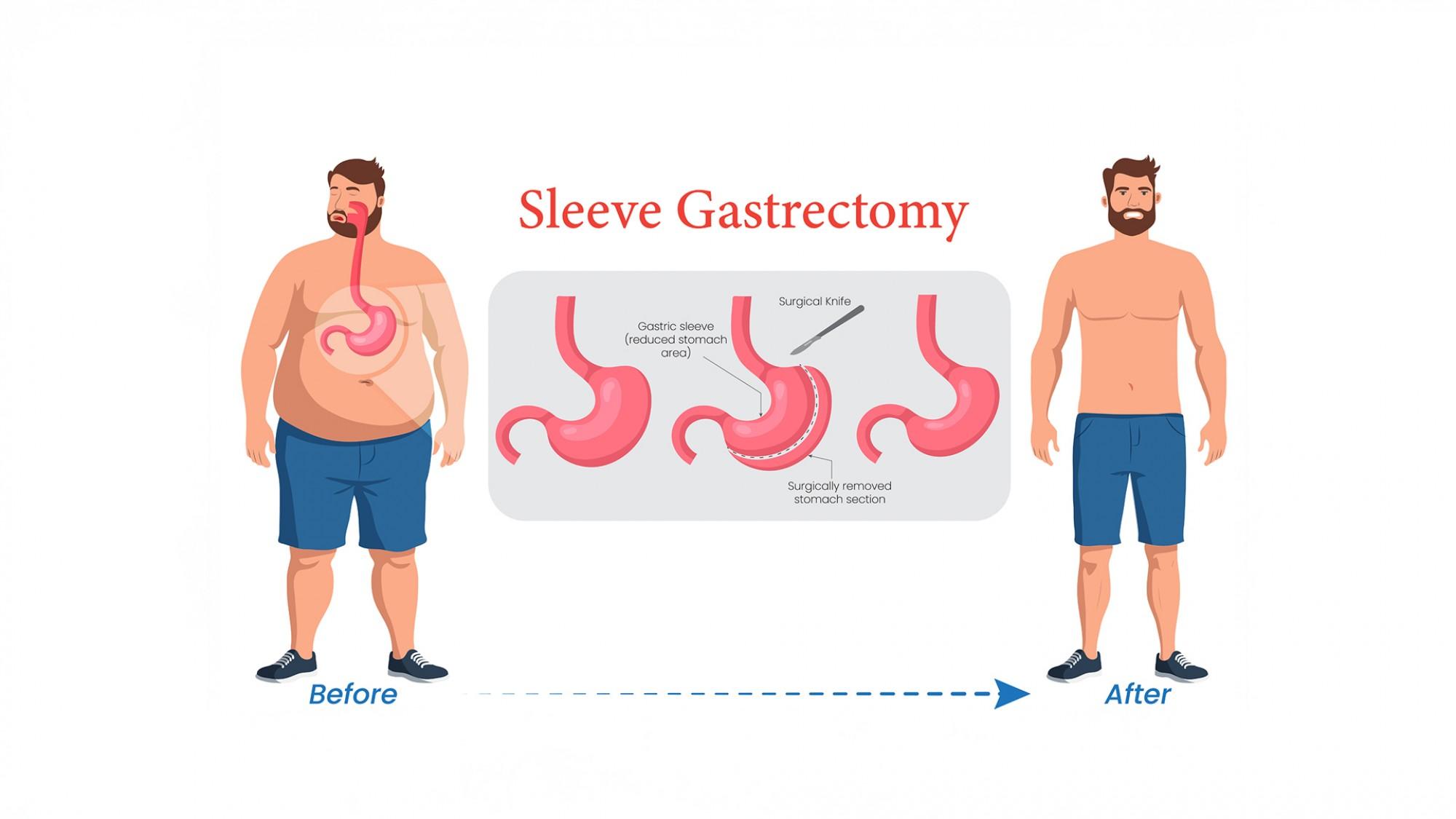
What Is Sleeve Gastrectomy?
Sleeve gastrectomy, often referred to as gastric sleeve surgery or surgical sleeve, involves removing about 75–80% of the stomach. What remains is a narrow "sleeve"-shaped tube that significantly reduces the amount of food you can eat and alters hunger hormones like ghrelin.
This procedure is typically performed as a laparoscopic surgery (or lapo surgery), which uses keyhole surgery techniques for smaller incisions, less pain, and quicker recovery.
Who Is a Good Candidate for Bariatric Surgery?
Not everyone with excess weight qualifies for bariatric surgery. You may be eligible for a sleeve gastrectomy if:
-
Your BMI is over 40, or over 35 with health issues like diabetes, hypertension, or sleep apnea
-
You’ve tried and failed traditional weight-loss methods
-
You're committed to long-term lifestyle changes and follow-ups
-
You don’t have untreated psychological conditions or alcohol/substance abuse
This procedure is not just about weight loss. It’s about improving the quality of life and reducing the risks of chronic conditions.
How Is It Performed?
The surgery is performed under general anesthesia. Using laparoscopy, the surgeon makes 4–5 small incisions and inserts a camera and instruments to remove the majority of the stomach.
Unlike gastric bypass, the intestines remain untouched. This reduces the risk of nutritional deficiencies.
Key points:
-
Surgery time: 1–2 hours
-
Hospital stay: 1–2 days
-
Recovery: 2–4 weeks
-
Scarring: Minimal, due to keyhole incisions
-
Pain: Managed with post-op medications
The laparoscopic approach significantly shortens the healing process compared to open surgery.
Life After Sleeve Gastrectomy
Post-op recovery involves several dietary stages:
-
Clear liquids for the first few days
-
Pureed foods for 2–3 weeks
-
Soft solids for a few more weeks
-
Gradual transition to regular, smaller meals
Most patients lose 50–70% of excess weight within 12–18 months. Common benefits include:
-
Improved insulin resistance
-
Normalized blood pressure
-
Reduced joint pain
-
Increased energy and mobility
Many patients undergoing gastric sleeve previously had appendectomy, cholecystectomy, or even lap nissen fundoplication — proving that laparoscopic surgery can be safely repeated or combined when necessary.
Risks to Be Aware Of
While laparoscopic sleeve gastrectomy is generally safe, like all surgeries, it carries potential risks:
-
Bleeding or infection
-
Leakage from the staple line
-
Acid reflux (though often improved long-term)
-
Nutritional deficiencies if dietary guidelines aren’t followed
Your surgeon may recommend supplements and regular labs post-surgery.
Bariatric surgery, especially sleeve gastrectomy, is not a shortcut — it's a medically supervised path to long-term health and well-being. If you’ve tried diets, medication, or other therapies without sustained success, this minimally invasive, effective procedure might be the answer.
Consult a general surgeon or bariatric specialist for an evaluation and customized care plan. With tools like laparoscopic surgery, gastrectomy, and keyhole procedures, a healthier future may be just a few small incisions away.
When evaluating whether sleeve gastrectomy is right for you, it’s important to understand the financial aspect. Most reputable hospitals will provide comprehensive packages including surgery, hospital stay, pre-op assessments, and follow-up visits.







 04 406 3000
04 406 3000  04 406 3000
04 406 3000









