Vitrectomy Referral / Coordination
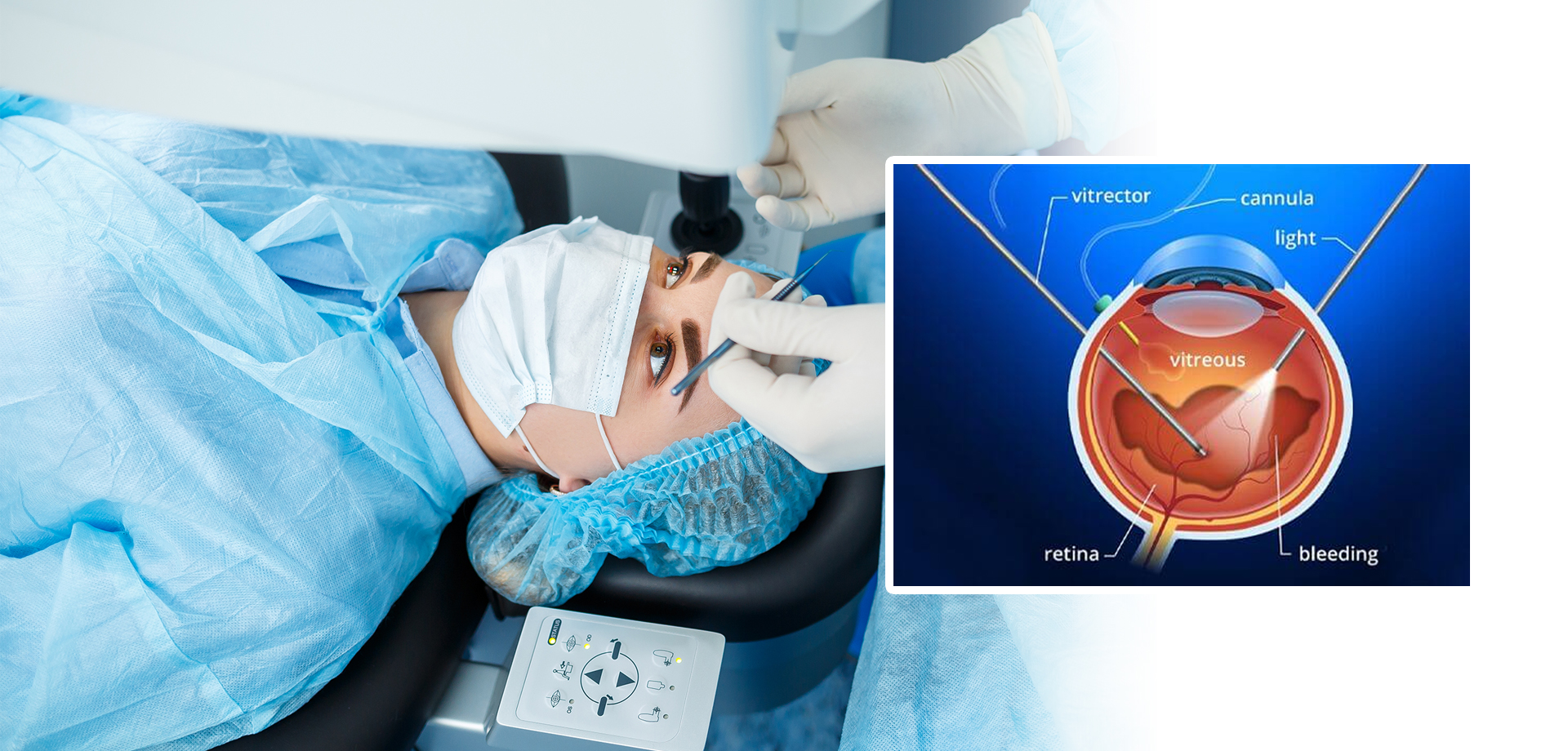
Vitrectomy referral and coordination is a critical component of comprehensive retinal care, particularly for patients with complex or vision-threatening vitreoretinal conditions that require advanced surgical intervention. A vitrectomy is a specialized microsurgical procedure in which the vitreous gel—the clear, jelly-like substance filling the eye—is removed to allow access to the retina and facilitate treatment of underlying retinal pathology. Because vitrectomy often involves highly specialized surgical expertise, sophisticated equipment, and multidisciplinary planning, effective referral and coordination play a pivotal role in patient outcomes.
Patients may require vitrectomy for a wide range of conditions, including retinal detachment, non-resolving vitreous hemorrhage, advanced diabetic retinopathy, macular hole, epiretinal membrane, endophthalmitis, and complications following eye trauma or previous eye surgery. In many cases, timely referral is vision-saving. Delays in diagnosis or coordination can result in irreversible retinal damage and permanent visual loss.
Vitrectomy referral begins with accurate identification of surgical indications during a comprehensive ophthalmic evaluation. Detailed documentation of symptoms, duration, visual acuity, retinal findings, and imaging results such as optical coherence tomography (OCT) and fundus photography are essential. Clear communication between the referring ophthalmologist and the vitreoretinal surgeon ensures that the receiving specialist has a complete understanding of disease severity and urgency.
Coordination extends beyond clinical handover. It involves patient counseling, appointment scheduling, insurance approvals, preoperative investigations, and postoperative follow-up planning. Many patients undergoing vitrectomy have systemic conditions such as diabetes or hypertension, requiring coordination with physicians to optimize medical stability prior to surgery. Educating patients about the procedure, expected outcomes, recovery timeline, and potential risks helps reduce anxiety and improve compliance.
Post-vitrectomy care is equally important. Patients often require positioning, medication adherence, activity modification, and close follow-up to monitor healing and detect complications such as infection, elevated eye pressure, cataract formation, or recurrent retinal detachment. Coordinated postoperative communication ensures continuity of care between the surgical center and the primary ophthalmology team.
A structured vitrectomy referral and coordination pathway improves efficiency, reduces delays, and enhances patient experience. By integrating diagnostics, counseling, surgical expertise, and follow-up care, this service ensures that patients receive timely, seamless, and high-quality retinal surgical management when it matters most.
Patients may require vitrectomy for a wide range of conditions, including retinal detachment, non-resolving vitreous hemorrhage, advanced diabetic retinopathy, macular hole, epiretinal membrane, endophthalmitis, and complications following eye trauma or previous eye surgery. In many cases, timely referral is vision-saving. Delays in diagnosis or coordination can result in irreversible retinal damage and permanent visual loss.
Vitrectomy referral begins with accurate identification of surgical indications during a comprehensive ophthalmic evaluation. Detailed documentation of symptoms, duration, visual acuity, retinal findings, and imaging results such as optical coherence tomography (OCT) and fundus photography are essential. Clear communication between the referring ophthalmologist and the vitreoretinal surgeon ensures that the receiving specialist has a complete understanding of disease severity and urgency.
Coordination extends beyond clinical handover. It involves patient counseling, appointment scheduling, insurance approvals, preoperative investigations, and postoperative follow-up planning. Many patients undergoing vitrectomy have systemic conditions such as diabetes or hypertension, requiring coordination with physicians to optimize medical stability prior to surgery. Educating patients about the procedure, expected outcomes, recovery timeline, and potential risks helps reduce anxiety and improve compliance.
Post-vitrectomy care is equally important. Patients often require positioning, medication adherence, activity modification, and close follow-up to monitor healing and detect complications such as infection, elevated eye pressure, cataract formation, or recurrent retinal detachment. Coordinated postoperative communication ensures continuity of care between the surgical center and the primary ophthalmology team.
A structured vitrectomy referral and coordination pathway improves efficiency, reduces delays, and enhances patient experience. By integrating diagnostics, counseling, surgical expertise, and follow-up care, this service ensures that patients receive timely, seamless, and high-quality retinal surgical management when it matters most.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









