Spinal Anesthesia
Spinal anesthesia is a form of regional anesthesia that produces rapid, profound, and predictable anesthesia of the lower half of the body by injecting a local anesthetic into the subarachnoid space of the spinal canal. It is widely used for surgeries involving the lower abdomen, pelvis, and lower limbs and is particularly common in obstetrics, orthopedic procedures, and urologic surgeries. Spinal anesthesia allows patients to remain awake while achieving complete sensory and motor blockade below a specific spinal level.
The procedure begins with a thorough pre-anesthetic evaluation to assess patient suitability, medical history, medications, coagulation status, and spinal anatomy. Contraindications such as infection at the injection site, bleeding disorders, or patient refusal are carefully ruled out. Patient counseling is essential to explain the expected effects, duration, and sensations associated with spinal anesthesia.
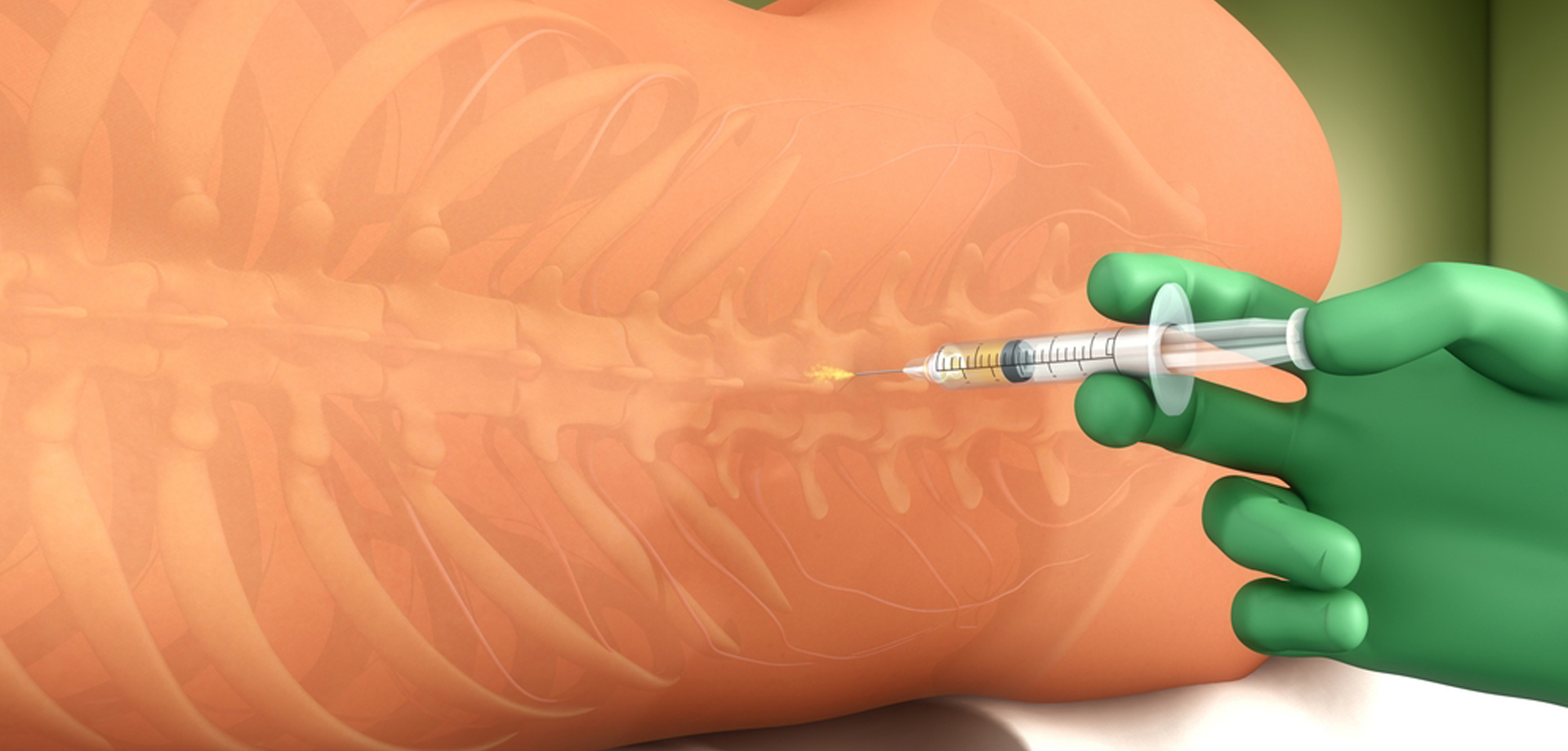
Spinal anesthesia is administered by inserting a fine needle into the lower lumbar region, below the termination of the spinal cord, and injecting a small volume of local anesthetic into the cerebrospinal fluid. This produces rapid onset anesthesia, typically within minutes, resulting in loss of sensation, muscle relaxation, and sympathetic blockade. The level and duration of anesthesia depend on the drug used, dose, and patient positioning.
One of the key advantages of spinal anesthesia is its reliability and rapid onset. It provides excellent surgical conditions, minimal drug exposure, and reduced stress response compared to general anesthesia. Patients maintain spontaneous breathing, avoiding airway manipulation and reducing respiratory risks. These features make spinal anesthesia particularly valuable for elderly patients and those with underlying cardiopulmonary disease.
Spinal anesthesia is extensively used in obstetric practice, especially for cesarean section, due to its rapid onset, dense sensory block, and minimal fetal drug exposure. It allows mothers to remain awake and alert during delivery while providing effective pain relief and muscle relaxation.
Potential side effects include low blood pressure due to sympathetic blockade, nausea, headache, and transient neurological symptoms. Post-dural puncture headache is a recognized complication but occurs infrequently with modern fine-gauge needles. Careful technique, appropriate fluid management, and vigilant monitoring significantly reduce complication risk.
Post-procedure care focuses on monitoring vital signs, motor recovery, and pain control as the anesthetic wears off. Most patients recover full sensation and mobility within a few hours.
Spinal anesthesia remains a cornerstone of regional anesthesia practice, offering predictable anesthesia, excellent pain control, and high patient satisfaction when administered by experienced anesthesia professionals.
The procedure begins with a thorough pre-anesthetic evaluation to assess patient suitability, medical history, medications, coagulation status, and spinal anatomy. Contraindications such as infection at the injection site, bleeding disorders, or patient refusal are carefully ruled out. Patient counseling is essential to explain the expected effects, duration, and sensations associated with spinal anesthesia.
Spinal anesthesia is administered by inserting a fine needle into the lower lumbar region, below the termination of the spinal cord, and injecting a small volume of local anesthetic into the cerebrospinal fluid. This produces rapid onset anesthesia, typically within minutes, resulting in loss of sensation, muscle relaxation, and sympathetic blockade. The level and duration of anesthesia depend on the drug used, dose, and patient positioning.
One of the key advantages of spinal anesthesia is its reliability and rapid onset. It provides excellent surgical conditions, minimal drug exposure, and reduced stress response compared to general anesthesia. Patients maintain spontaneous breathing, avoiding airway manipulation and reducing respiratory risks. These features make spinal anesthesia particularly valuable for elderly patients and those with underlying cardiopulmonary disease.
Spinal anesthesia is extensively used in obstetric practice, especially for cesarean section, due to its rapid onset, dense sensory block, and minimal fetal drug exposure. It allows mothers to remain awake and alert during delivery while providing effective pain relief and muscle relaxation.
Potential side effects include low blood pressure due to sympathetic blockade, nausea, headache, and transient neurological symptoms. Post-dural puncture headache is a recognized complication but occurs infrequently with modern fine-gauge needles. Careful technique, appropriate fluid management, and vigilant monitoring significantly reduce complication risk.
Post-procedure care focuses on monitoring vital signs, motor recovery, and pain control as the anesthetic wears off. Most patients recover full sensation and mobility within a few hours.
Spinal anesthesia remains a cornerstone of regional anesthesia practice, offering predictable anesthesia, excellent pain control, and high patient satisfaction when administered by experienced anesthesia professionals.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









