Whipple Procedure (Pancreaticoduodenectomy)
The Whipple procedure, medically known as pancreaticoduodenectomy, is a complex and highly specialized gastrointestinal surgery performed to treat diseases affecting the pancreas, bile duct, duodenum, and surrounding structures. It is most commonly indicated for cancers of the pancreatic head, distal bile duct, ampulla of Vater, and duodenum. Due to the anatomical complexity and critical functions of the involved organs, the Whipple procedure requires advanced surgical expertise, meticulous planning, and comprehensive postoperative care.
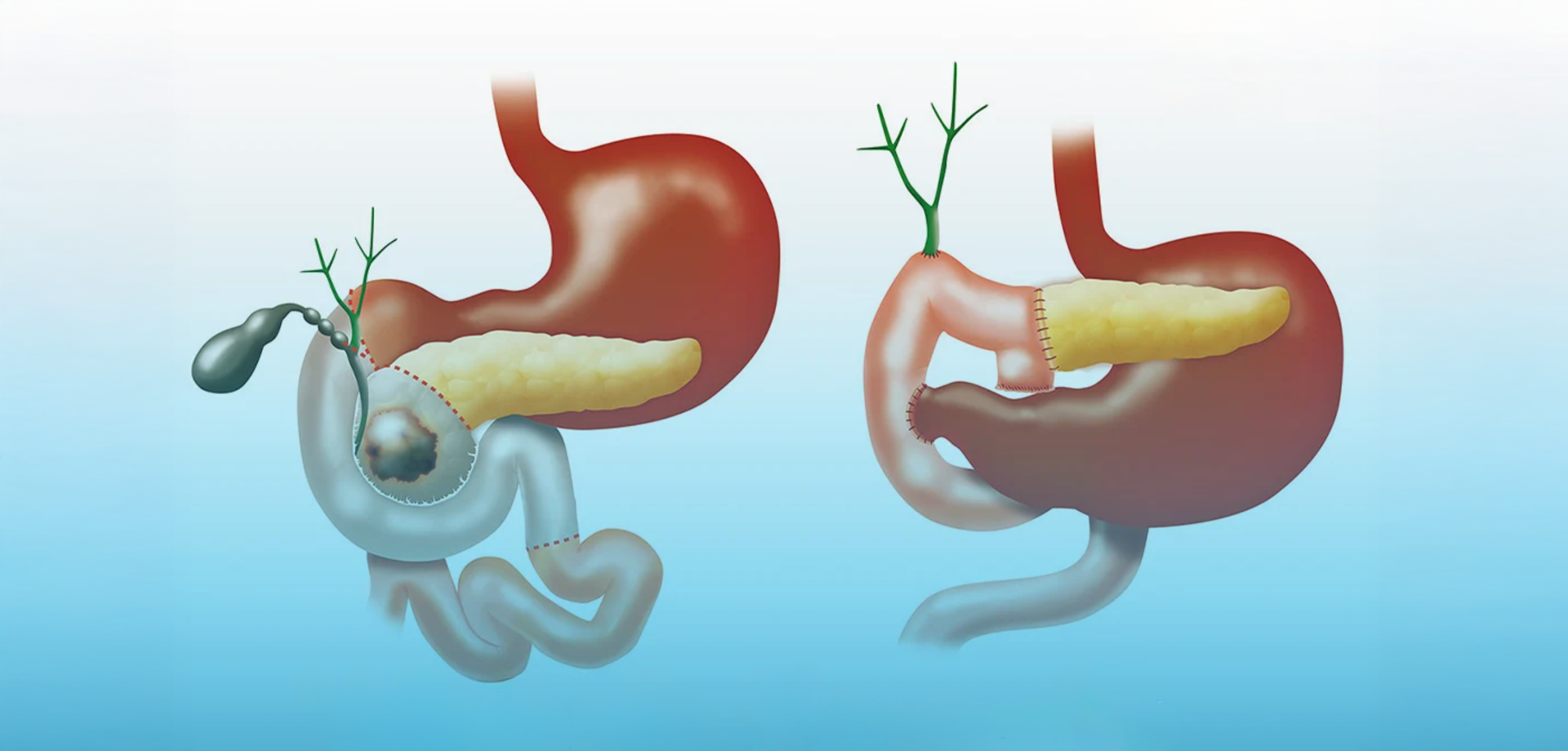
The pancreas plays a central role in digestion and blood sugar regulation, while the duodenum is the first part of the small intestine and closely linked to the bile duct and stomach. In conditions such as pancreatic cancer, tumors often arise near these interconnected structures, necessitating removal of multiple organs in a single operation. The Whipple procedure involves removal of the head of the pancreas, part of the small intestine (duodenum), the gallbladder, a portion of the bile duct, and sometimes part of the stomach, followed by reconstruction to restore digestive continuity.
The Whipple procedure is primarily indicated for malignant tumors localized to the pancreatic head region that have not spread to distant organs. It may also be performed for selected benign or pre-malignant conditions such as chronic pancreatitis with complications, large pancreatic cysts, or neuroendocrine tumors. Careful patient selection is critical, as this is a major operation with significant physiological impact.
Preoperative evaluation is extensive and includes high-resolution CT or MRI scans, endoscopic ultrasound, blood tests, and assessment of nutritional and functional status. Multidisciplinary tumor board discussions involving GI surgeons, oncologists, radiologists, gastroenterologists, and anesthesiologists are essential to determine suitability and optimize outcomes. In cancer cases, neoadjuvant chemotherapy may be recommended prior to surgery.
The procedure is performed under general anesthesia in a specialized operating theater. Advances in surgical technique and perioperative care have significantly improved outcomes, reducing complication rates and mortality. In selected centers and patients, minimally invasive or robotic-assisted Whipple procedures may be performed, although open surgery remains standard in many cases.
Postoperative care focuses on intensive monitoring, pain management, nutritional support, and prevention of complications such as infection, delayed gastric emptying, or pancreatic leaks. Recovery requires a structured approach, with gradual reintroduction of oral intake and long-term follow-up to manage digestive enzyme supplementation and blood sugar control if needed.
The Whipple procedure offers the best chance for long-term survival in patients with localized pancreatic and periampullary cancers. When performed in experienced centers with multidisciplinary support, it provides meaningful extension of life, symptom relief, and improved quality of care for complex pancreatic diseases.
The pancreas plays a central role in digestion and blood sugar regulation, while the duodenum is the first part of the small intestine and closely linked to the bile duct and stomach. In conditions such as pancreatic cancer, tumors often arise near these interconnected structures, necessitating removal of multiple organs in a single operation. The Whipple procedure involves removal of the head of the pancreas, part of the small intestine (duodenum), the gallbladder, a portion of the bile duct, and sometimes part of the stomach, followed by reconstruction to restore digestive continuity.
The Whipple procedure is primarily indicated for malignant tumors localized to the pancreatic head region that have not spread to distant organs. It may also be performed for selected benign or pre-malignant conditions such as chronic pancreatitis with complications, large pancreatic cysts, or neuroendocrine tumors. Careful patient selection is critical, as this is a major operation with significant physiological impact.
Preoperative evaluation is extensive and includes high-resolution CT or MRI scans, endoscopic ultrasound, blood tests, and assessment of nutritional and functional status. Multidisciplinary tumor board discussions involving GI surgeons, oncologists, radiologists, gastroenterologists, and anesthesiologists are essential to determine suitability and optimize outcomes. In cancer cases, neoadjuvant chemotherapy may be recommended prior to surgery.
The procedure is performed under general anesthesia in a specialized operating theater. Advances in surgical technique and perioperative care have significantly improved outcomes, reducing complication rates and mortality. In selected centers and patients, minimally invasive or robotic-assisted Whipple procedures may be performed, although open surgery remains standard in many cases.
Postoperative care focuses on intensive monitoring, pain management, nutritional support, and prevention of complications such as infection, delayed gastric emptying, or pancreatic leaks. Recovery requires a structured approach, with gradual reintroduction of oral intake and long-term follow-up to manage digestive enzyme supplementation and blood sugar control if needed.
The Whipple procedure offers the best chance for long-term survival in patients with localized pancreatic and periampullary cancers. When performed in experienced centers with multidisciplinary support, it provides meaningful extension of life, symptom relief, and improved quality of care for complex pancreatic diseases.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









