Gastrectomy (Partial or Total)
Gastrectomy is a major gastrointestinal surgical procedure involving the partial or complete removal of the stomach. It is performed to treat a range of serious gastric conditions, most commonly gastric cancer, severe peptic ulcer disease with complications, and certain non-cancerous gastric tumors. Because the stomach plays a critical role in digestion and nutrient absorption, gastrectomy requires meticulous surgical planning, expert execution, and comprehensive postoperative care.
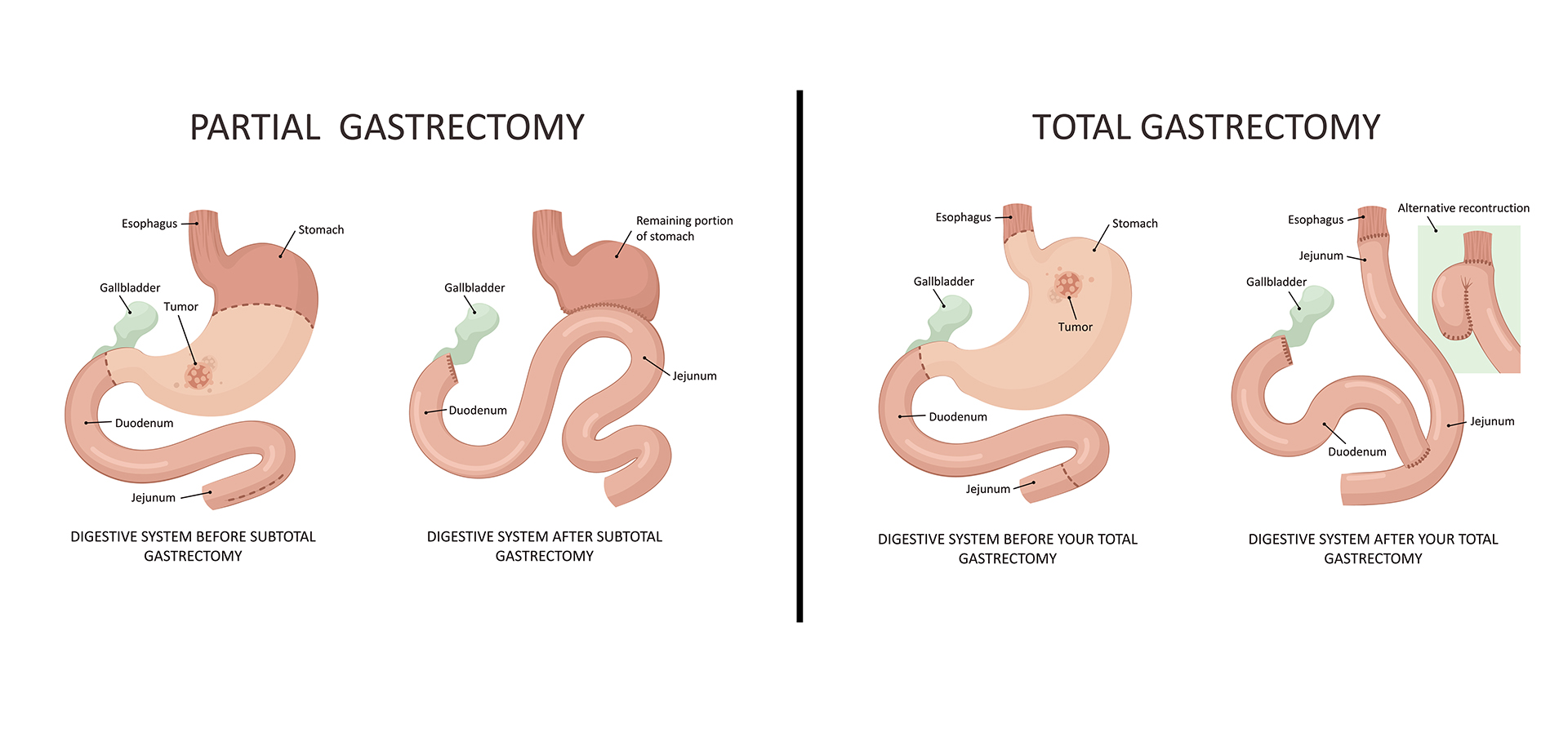
A partial gastrectomy involves removal of the diseased portion of the stomach while preserving the remaining healthy tissue. This approach is commonly used for localized gastric tumors or complicated ulcers confined to a specific area. A total gastrectomy, in contrast, involves complete removal of the stomach and reconstruction of the digestive tract by connecting the esophagus directly to the small intestine. The choice between partial and total gastrectomy depends on disease extent, location, pathology, and patient factors.
Gastrectomy is primarily indicated in patients with gastric cancer, particularly when the disease is localized and potentially curable through surgery. It is also indicated in cases of severe or recurrent gastric ulcers that do not respond to medical therapy, bleeding ulcers, gastric perforation, and certain inherited cancer syndromes. Preoperative evaluation includes endoscopy with biopsy, CT or PET imaging, nutritional assessment, and multidisciplinary tumor board review when cancer is suspected.
The procedure is performed under general anesthesia in a specialized operating theater. Advances in surgical techniques have enabled many gastrectomies to be performed using minimally invasive laparoscopic or robotic approaches in selected patients. These techniques reduce blood loss, postoperative pain, and recovery time while maintaining oncological safety. Open gastrectomy remains necessary in advanced or complex cases.
Following gastrectomy, reconstruction of the digestive tract is carefully performed to allow food passage and nutrient absorption. Postoperative care focuses on pain management, nutritional support, early mobilization, and monitoring for complications such as leaks, infection, or nutritional deficiencies. Patients require gradual dietary progression and long-term nutritional follow-up, including vitamin and mineral supplementation when needed.
Gastrectomy significantly improves survival in appropriately selected gastric cancer patients and provides definitive treatment for severe gastric disease. With expert surgical care and structured follow-up, patients can adapt well to dietary changes and maintain good quality of life after surgery.
A partial gastrectomy involves removal of the diseased portion of the stomach while preserving the remaining healthy tissue. This approach is commonly used for localized gastric tumors or complicated ulcers confined to a specific area. A total gastrectomy, in contrast, involves complete removal of the stomach and reconstruction of the digestive tract by connecting the esophagus directly to the small intestine. The choice between partial and total gastrectomy depends on disease extent, location, pathology, and patient factors.
Gastrectomy is primarily indicated in patients with gastric cancer, particularly when the disease is localized and potentially curable through surgery. It is also indicated in cases of severe or recurrent gastric ulcers that do not respond to medical therapy, bleeding ulcers, gastric perforation, and certain inherited cancer syndromes. Preoperative evaluation includes endoscopy with biopsy, CT or PET imaging, nutritional assessment, and multidisciplinary tumor board review when cancer is suspected.
The procedure is performed under general anesthesia in a specialized operating theater. Advances in surgical techniques have enabled many gastrectomies to be performed using minimally invasive laparoscopic or robotic approaches in selected patients. These techniques reduce blood loss, postoperative pain, and recovery time while maintaining oncological safety. Open gastrectomy remains necessary in advanced or complex cases.
Following gastrectomy, reconstruction of the digestive tract is carefully performed to allow food passage and nutrient absorption. Postoperative care focuses on pain management, nutritional support, early mobilization, and monitoring for complications such as leaks, infection, or nutritional deficiencies. Patients require gradual dietary progression and long-term nutritional follow-up, including vitamin and mineral supplementation when needed.
Gastrectomy significantly improves survival in appropriately selected gastric cancer patients and provides definitive treatment for severe gastric disease. With expert surgical care and structured follow-up, patients can adapt well to dietary changes and maintain good quality of life after surgery.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









