GI Stenting
Gastrointestinal (GI) stenting is a minimally invasive endoscopic procedure used to relieve obstruction within the digestive tract caused by benign or malignant conditions. Obstruction can occur at various levels of the gastrointestinal system, including the esophagus, stomach, small intestine, colon, or bile ducts, and may significantly impair a patient’s ability to eat, digest, or eliminate waste. GI stenting plays a crucial role in restoring luminal patency, relieving symptoms, and improving quality of life without the need for major surgery.
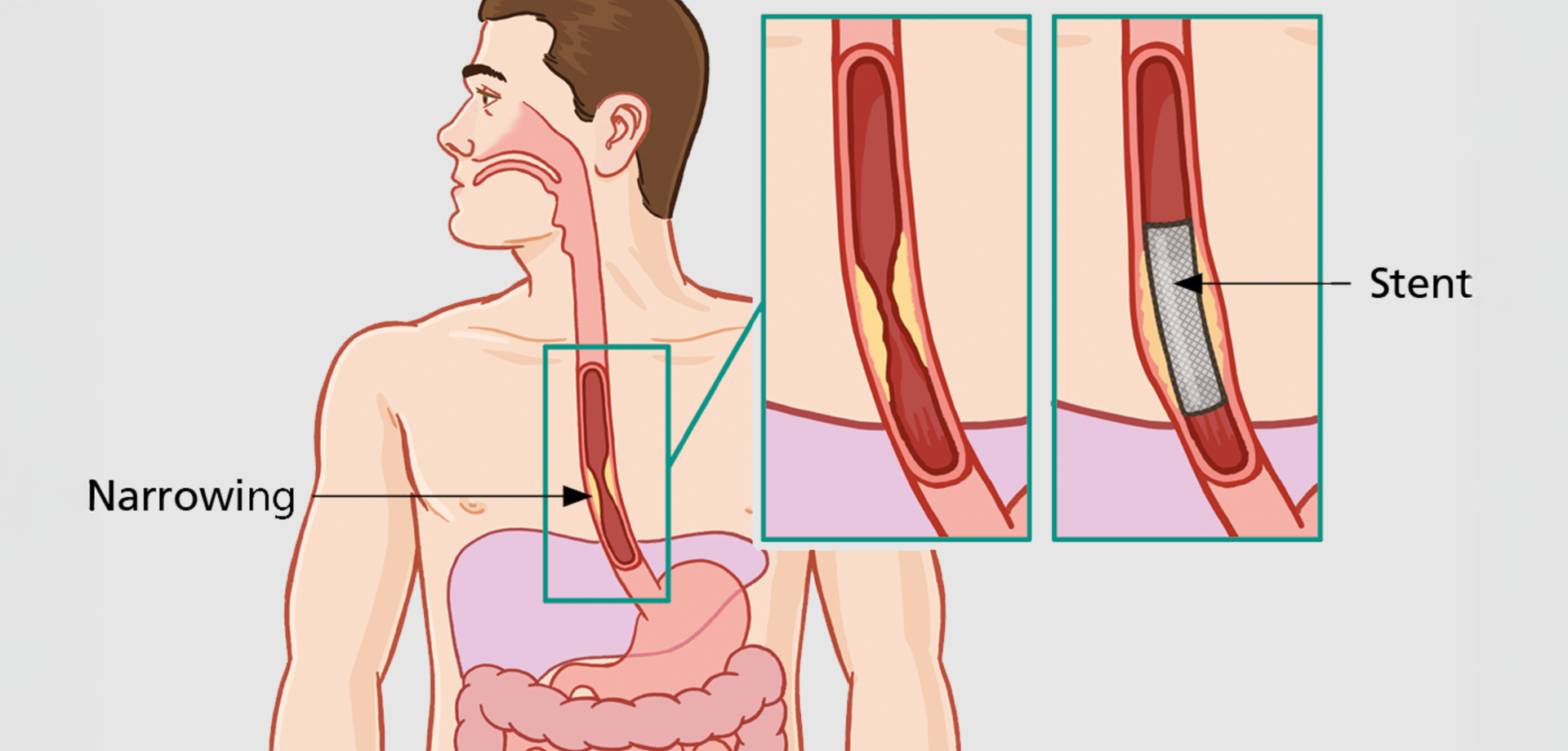
The procedure involves placement of a stent, which is a small, expandable mesh tube designed to hold open a narrowed or blocked segment of the gastrointestinal tract. Stents are typically made of metal or polymer and are inserted endoscopically under imaging guidance. Once deployed, the stent expands to restore the normal passage of food, fluids, or bile, depending on the location of the obstruction.
GI stenting is commonly indicated in conditions such as esophageal strictures, esophageal cancer causing difficulty swallowing, gastric outlet obstruction, colonic obstruction due to tumors, and bile duct blockage leading to jaundice. It is particularly valuable for patients who are not suitable candidates for surgery due to advanced disease, medical comorbidities, or poor overall health. In many cases, GI stenting provides rapid symptom relief and allows patients to resume oral intake shortly after the procedure.
The procedure is performed using endoscopic techniques, often combined with fluoroscopic imaging for precise placement. Under sedation, an endoscope is advanced to the site of obstruction, and the stent is positioned across the narrowed segment. Once released, the stent expands gradually, restoring patency while maintaining flexibility to accommodate natural movement of the digestive tract. The procedure is typically completed within a short time frame and does not require surgical incisions.
GI stenting can be used for both palliative and therapeutic purposes. In malignant conditions, stenting provides effective palliation by relieving obstruction-related symptoms, improving nutrition, and reducing hospital admissions. In benign conditions, stents may be placed temporarily to allow healing or as a bridge to definitive surgery. The choice of stent type and duration depends on the underlying condition and treatment goals.
Following stent placement, patients are monitored to ensure adequate symptom relief and early detection of complications such as migration, blockage, or bleeding, which are relatively uncommon when the procedure is performed by experienced specialists. Dietary advice and follow-up assessments are provided to optimize outcomes and ensure stent function.
GI stenting has become an integral part of modern gastroenterology and interventional endoscopy. By offering a safe, effective, and minimally invasive solution to gastrointestinal obstruction, it reduces the need for emergency surgery, shortens hospital stays, and significantly improves patient comfort and functional status. When used in appropriately selected patients, GI stenting delivers meaningful clinical benefit and supports comprehensive digestive care.
The procedure involves placement of a stent, which is a small, expandable mesh tube designed to hold open a narrowed or blocked segment of the gastrointestinal tract. Stents are typically made of metal or polymer and are inserted endoscopically under imaging guidance. Once deployed, the stent expands to restore the normal passage of food, fluids, or bile, depending on the location of the obstruction.
GI stenting is commonly indicated in conditions such as esophageal strictures, esophageal cancer causing difficulty swallowing, gastric outlet obstruction, colonic obstruction due to tumors, and bile duct blockage leading to jaundice. It is particularly valuable for patients who are not suitable candidates for surgery due to advanced disease, medical comorbidities, or poor overall health. In many cases, GI stenting provides rapid symptom relief and allows patients to resume oral intake shortly after the procedure.
The procedure is performed using endoscopic techniques, often combined with fluoroscopic imaging for precise placement. Under sedation, an endoscope is advanced to the site of obstruction, and the stent is positioned across the narrowed segment. Once released, the stent expands gradually, restoring patency while maintaining flexibility to accommodate natural movement of the digestive tract. The procedure is typically completed within a short time frame and does not require surgical incisions.
GI stenting can be used for both palliative and therapeutic purposes. In malignant conditions, stenting provides effective palliation by relieving obstruction-related symptoms, improving nutrition, and reducing hospital admissions. In benign conditions, stents may be placed temporarily to allow healing or as a bridge to definitive surgery. The choice of stent type and duration depends on the underlying condition and treatment goals.
Following stent placement, patients are monitored to ensure adequate symptom relief and early detection of complications such as migration, blockage, or bleeding, which are relatively uncommon when the procedure is performed by experienced specialists. Dietary advice and follow-up assessments are provided to optimize outcomes and ensure stent function.
GI stenting has become an integral part of modern gastroenterology and interventional endoscopy. By offering a safe, effective, and minimally invasive solution to gastrointestinal obstruction, it reduces the need for emergency surgery, shortens hospital stays, and significantly improves patient comfort and functional status. When used in appropriately selected patients, GI stenting delivers meaningful clinical benefit and supports comprehensive digestive care.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









