ERCP (Endoscopic Retrograde Cholangiopancreatography)
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a highly specialized endoscopic procedure used to diagnose and treat disorders of the bile ducts, pancreatic ducts, and gallbladder. It combines endoscopy with fluoroscopic X-ray imaging, allowing both visualization and therapeutic intervention within the hepatobiliary and pancreatic systems. ERCP is an advanced procedure typically performed in tertiary care centers by experienced gastroenterologists.
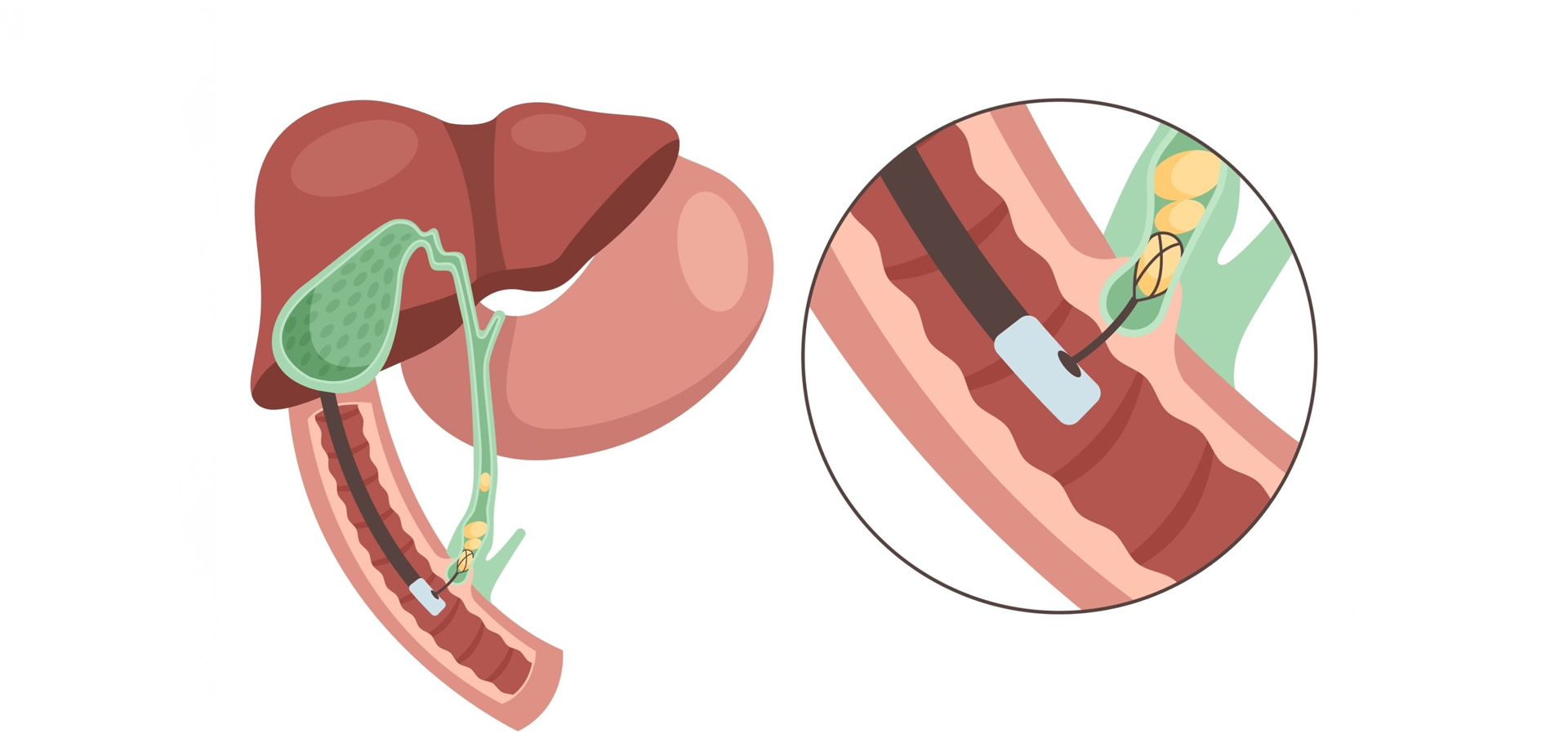
The procedure involves advancing a flexible endoscope through the mouth, esophagus, and stomach into the duodenum, where the bile and pancreatic ducts open. A contrast dye is injected into these ducts under X-ray guidance, enabling detailed imaging of ductal anatomy. This allows identification of blockages, stones, strictures, leaks, or tumors affecting the biliary or pancreatic system.
ERCP is primarily indicated for therapeutic rather than purely diagnostic purposes. Common indications include bile duct stones causing jaundice or infection, narrowing or obstruction of bile ducts, recurrent pancreatitis due to ductal blockage, bile leaks following surgery, and suspected cancers of the bile ducts or pancreas. In many cases, ERCP allows definitive treatment without the need for open surgery.
One of the key benefits of ERCP is the ability to perform immediate interventions during the same procedure. These include removal of bile duct stones, widening of narrowed ducts through sphincterotomy, and placement of biliary or pancreatic stents to restore normal drainage. These interventions provide rapid symptom relief and prevent serious complications such as infection, liver damage, or pancreatitis.
ERCP is performed under deep sedation or general anesthesia in a controlled environment with continuous monitoring. Advanced imaging and specialized instruments ensure precision and safety. Although ERCP carries a higher risk profile compared to standard endoscopy, careful patient selection and expert technique significantly reduce complications.
Following the procedure, patients are closely monitored for a short period to ensure safe recovery. Most patients experience significant improvement in symptoms once ductal obstruction is relieved. Long-term follow-up may be required depending on the underlying condition and whether stents have been placed.
ERCP plays a crucial role in modern gastroenterology by providing minimally invasive solutions to complex biliary and pancreatic disorders. When performed in appropriately selected patients, it improves outcomes, reduces hospital stays, and avoids the need for major surgical intervention.
The procedure involves advancing a flexible endoscope through the mouth, esophagus, and stomach into the duodenum, where the bile and pancreatic ducts open. A contrast dye is injected into these ducts under X-ray guidance, enabling detailed imaging of ductal anatomy. This allows identification of blockages, stones, strictures, leaks, or tumors affecting the biliary or pancreatic system.
ERCP is primarily indicated for therapeutic rather than purely diagnostic purposes. Common indications include bile duct stones causing jaundice or infection, narrowing or obstruction of bile ducts, recurrent pancreatitis due to ductal blockage, bile leaks following surgery, and suspected cancers of the bile ducts or pancreas. In many cases, ERCP allows definitive treatment without the need for open surgery.
One of the key benefits of ERCP is the ability to perform immediate interventions during the same procedure. These include removal of bile duct stones, widening of narrowed ducts through sphincterotomy, and placement of biliary or pancreatic stents to restore normal drainage. These interventions provide rapid symptom relief and prevent serious complications such as infection, liver damage, or pancreatitis.
ERCP is performed under deep sedation or general anesthesia in a controlled environment with continuous monitoring. Advanced imaging and specialized instruments ensure precision and safety. Although ERCP carries a higher risk profile compared to standard endoscopy, careful patient selection and expert technique significantly reduce complications.
Following the procedure, patients are closely monitored for a short period to ensure safe recovery. Most patients experience significant improvement in symptoms once ductal obstruction is relieved. Long-term follow-up may be required depending on the underlying condition and whether stents have been placed.
ERCP plays a crucial role in modern gastroenterology by providing minimally invasive solutions to complex biliary and pancreatic disorders. When performed in appropriately selected patients, it improves outcomes, reduces hospital stays, and avoids the need for major surgical intervention.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









