Peripheral Angiography & Angioplasty
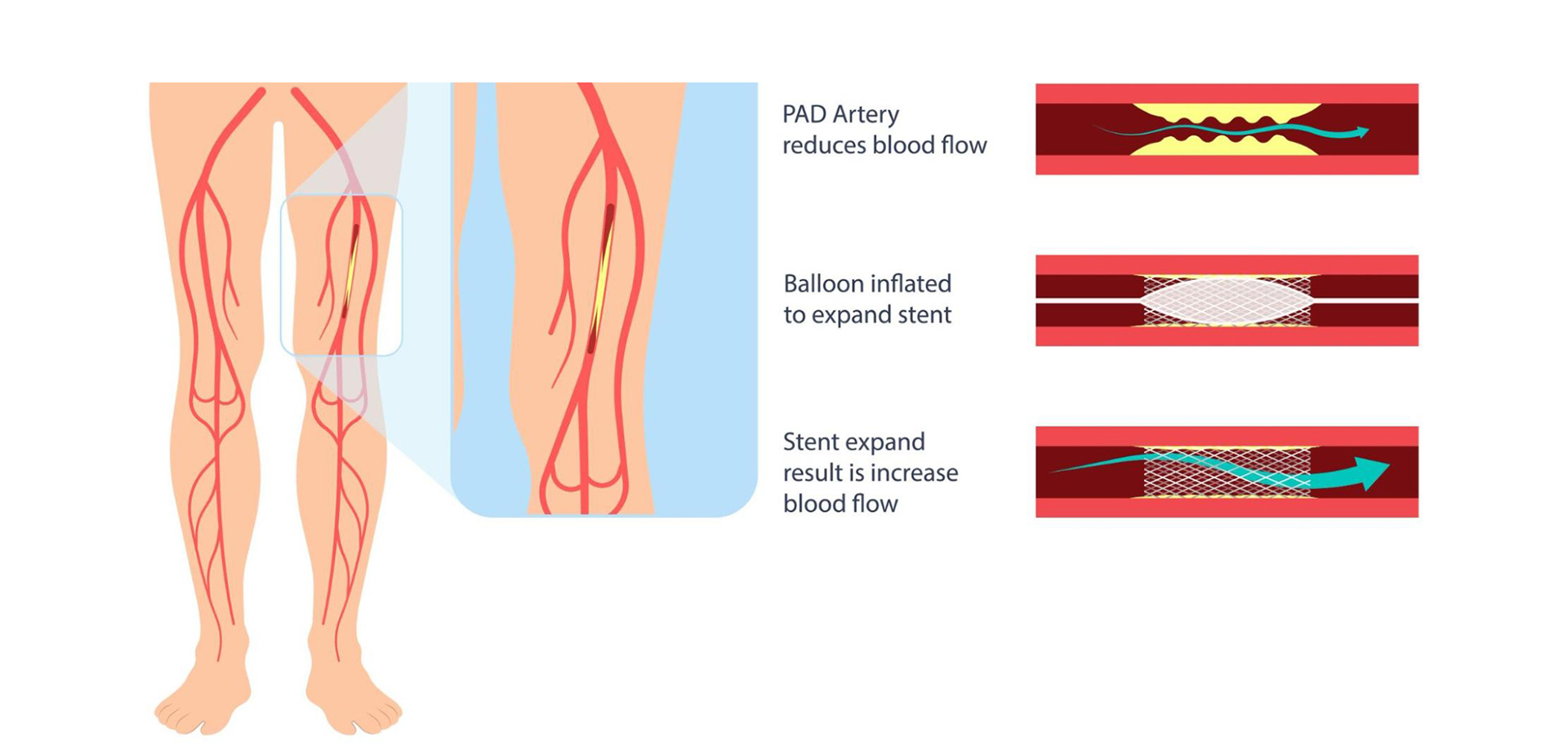
Peripheral angiography and angioplasty are specialized vascular interventions used to diagnose and treat narrowing or blockages in arteries supplying blood to the limbs, most commonly the legs. These conditions fall under peripheral arterial disease (PAD), a progressive atherosclerotic disorder that reduces blood flow and can significantly impair mobility, wound healing, and limb viability if left untreated.
Patients with peripheral arterial disease may present with leg pain while walking (claudication), numbness, cold extremities, non-healing ulcers, or discoloration of the skin. In advanced stages, reduced blood supply can lead to critical limb ischemia, increasing the risk of infection, tissue loss, or amputation. Early diagnosis and timely vascular intervention are essential to prevent disease progression.
Peripheral angiography is a diagnostic procedure that uses catheter-based imaging to visualize blood flow through peripheral arteries. It allows precise identification of arterial narrowing, blockages, or anatomical abnormalities. The diagnostic findings guide treatment planning and determine whether angioplasty is required.
Peripheral angioplasty is a minimally invasive procedure performed to restore blood flow by widening the narrowed artery. Using catheter-based techniques, the affected segment is treated to improve circulation and relieve ischemic symptoms. Angioplasty improves walking capacity, promotes healing of ulcers, and enhances overall limb function.
These procedures are performed in a specialized vascular catheterization laboratory by experienced interventional cardiologists or vascular specialists. Continuous imaging guidance ensures accurate treatment while minimizing risk to surrounding vessels. The minimally invasive nature of angioplasty allows faster recovery, reduced hospital stay, and lower complication rates compared to open surgical procedures.
Peripheral angiography and angioplasty are particularly beneficial for patients with diabetes, smoking history, hypertension, or chronic kidney disease, as these populations are at higher risk for PAD. Careful patient selection and individualized treatment planning are central to achieving optimal outcomes.
Post-procedure care includes monitoring of circulation, access-site care, and long-term vascular risk management. Patients benefit from structured follow-up to monitor symptom improvement and prevent disease recurrence. When integrated into comprehensive cardiovascular care, peripheral angioplasty significantly improves quality of life and limb preservation.
Patients with peripheral arterial disease may present with leg pain while walking (claudication), numbness, cold extremities, non-healing ulcers, or discoloration of the skin. In advanced stages, reduced blood supply can lead to critical limb ischemia, increasing the risk of infection, tissue loss, or amputation. Early diagnosis and timely vascular intervention are essential to prevent disease progression.
Peripheral angiography is a diagnostic procedure that uses catheter-based imaging to visualize blood flow through peripheral arteries. It allows precise identification of arterial narrowing, blockages, or anatomical abnormalities. The diagnostic findings guide treatment planning and determine whether angioplasty is required.
Peripheral angioplasty is a minimally invasive procedure performed to restore blood flow by widening the narrowed artery. Using catheter-based techniques, the affected segment is treated to improve circulation and relieve ischemic symptoms. Angioplasty improves walking capacity, promotes healing of ulcers, and enhances overall limb function.
These procedures are performed in a specialized vascular catheterization laboratory by experienced interventional cardiologists or vascular specialists. Continuous imaging guidance ensures accurate treatment while minimizing risk to surrounding vessels. The minimally invasive nature of angioplasty allows faster recovery, reduced hospital stay, and lower complication rates compared to open surgical procedures.
Peripheral angiography and angioplasty are particularly beneficial for patients with diabetes, smoking history, hypertension, or chronic kidney disease, as these populations are at higher risk for PAD. Careful patient selection and individualized treatment planning are central to achieving optimal outcomes.
Post-procedure care includes monitoring of circulation, access-site care, and long-term vascular risk management. Patients benefit from structured follow-up to monitor symptom improvement and prevent disease recurrence. When integrated into comprehensive cardiovascular care, peripheral angioplasty significantly improves quality of life and limb preservation.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7





 04 406 3000
04 406 3000  04 406 3000
04 406 3000









